Muscular Dystrophy
Description
What it is. Muscular dystrophy (MD) is a group of rare diseases. They cause muscle fibers to weaken and break down. MD affects the skeletal or voluntary muscles that control movement in the arms, legs and trunk. It also can affect the heart and other involuntary muscles, such as those in the gut. MD passes from parent to child (genetic) and gets worse over time (progressive).
Types of MD. There are nine major types of MD affecting people of all ages, from infancy to middle age or later. The two most common types of MD affect children:
- Duchenne muscular dystrophy (DMD)
- Becker muscular dystrophy (BMD)
Both DMD and BMD affect boys almost exclusively, but in rare cases can also affect girls.
Diagnosis. To diagnose MD, give the doctor a complete medical history for your child and the family. The doctor will perform a thorough physical examination of your child and may use laboratory tests to confirm diagnosis of MD.
Medical history: Tell the doctor if other family members have any signs or symptoms of MD. Be sure to mention if your child has any other health problems. Also, tell the doctor at what age the child achieved growth milestones, such as learning how to walk.
Physical exam: The doctor will want to see how your child stands up from a sitting position on the floor. Children with DMD use the "Gower's maneuver" to stand up. They start out on their hands and feet, planting their feet widely apart and pushing up their bottom first. Then, they use their hands to push up on their knees and thighs. (See illustration below.) The doctor will also want to watch your child walk. He or she may carefully test the child's muscles and nervous system.
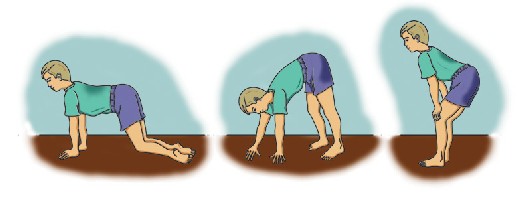
A child with DMD uses the Gower's maneuver to stand.
Lab tests: The doctor may use certain laboratory tests to be sure that your child has MD:
- Blood tests: The doctor checks a blood sample for high levels of the enzyme creatine kinase (CK). That can indicate muscle damage.
- Electromyography: The doctor puts small electrodes into muscle to measure electrical activity. Changes in the pattern of activity can show disease.
- Muscle biopsy: The doctor removes a small piece of muscle to study in the laboratory. This can distinguish various forms of MD from other muscle diseases.
- Genetic testing: In some cases, the doctor can study a blood sample to identify an abnormal gene and diagnose MD.
Coping with MD. Like all children, those with MD need to feel loved, valued and safe. They need to develop strong self-esteem. Parents, siblings, other family members and friends can help by seeing the child first, not the disease. Keep a positive attitude, communicate openly and honestly, and be patient and optimistic. By giving your love, support and encouragement, you can help the child have a happy and rewarding life, despite the challenges of MD. Some tips for coping:
- Encourage your child to stay independent for as long as possible.
- Answer your child's questions about MD. Give an older child more information about the disease, and allow him to take part in medical decision-making.
- Ask for and accept help from other people. Family members of people with MD face significant physical, emotional and financial commitments.
- Don't blame yourself for your child's MD. At various times, everyone in the family may experience all the stages of grief: denial, anger, bargaining, depression and acceptance. As MD progresses, crisis points can trigger powerful emotions. Consider joining a support group to learn coping strategies, and to know that you are not alone.
Symptoms
Both Duchenne and Becker muscular dystrophy cause weak muscles, lack of coordination and progressive disability.
Duchenne muscular dystrophy begins with muscle loss in the pelvis, upper arms and legs. The first signs and symptoms of DMD develop in young children aged 2 to 5. They may have:
- Difficulty walking, such as being late in learning how to walk (more than 18 months old), having a waddling gait or walking on toes or balls of the feet.
- Difficulty running or jumping caused by weakness in leg muscles.
- Frequent falls, stumbling and difficulty climbing stairs.
- Difficulty standing from a lying or sitting position.
- Reduced endurance.
- Enlarged calf muscles.
- Mild mental retardation, in some cases.
Becker muscular dystrophy begins with muscle loss in the hips, pelvis, thighs and shoulders. Becker is basically a milder form of Duchenne. Children with BMD may have:
- Difficulties similar to DMD.
- A waddling gait, perhaps walking on toes or sticking out the abdomen to balance weak muscles.
If you think your child may have MD, see your doctor as soon as possible for diagnosis and comprehensive care.
Risk Factors / Prevention
MD is a sex-linked recessive disease. It typically passes from a mother (who has no symptoms) to her son.
Treatment Options
Duchenne MD has a more certain and severe disease process than Becker MD. Doctors do not yet have a cure for any type of muscular dystrophy. Fortunately, timely interventions can help slow progression of complications and maximize your child's quality of life. When you are aware of what changes may come, you can watch for them and prepare any needed adjustments.
Duchenne: Many children with DMD lose their ability to walk by late childhood, and require wheelchairs. As muscles continue to weaken in the back and chest, they cannot hold their bodies upright, and most develop curvature of the spine (scoliosis). By the time they are teenagers, DMD usually progresses to weaken heart and respiratory muscles. Breathing problems eventually cause most people with DMD to die by their late teens or early 20s.
Becker: BMD progresses more slowly over the course of decades, and is a milder and less predictable disease. Some men with BMD need wheelchairs by age 30 or later; others manage for many years with minor aids, such as a walking cane.
Orthopaedic treatments. Goals in orthopaedic treatment of muscular dystrophy include keeping your child's body flexible, upright and mobile, and helping the child function independently for as long as possible. The doctor may recommend various treatments:
- Physical therapy and bracing to prevent contractures: The doctor may prescribe daily stretching exercises to improve a child's ability to walk. Regular, moderate physical therapy may help keep a range of motion in stiff or "frozen" joints. Walking braces for the ankle-foot or the knee-ankle-foot can help support weak muscles and keep the body flexible, slowing progression of contractures.
- Medications: Sometimes a doctor may prescribe anti-inflammatory corticosteroid medications to improve muscle strength and delay progression of DMD. (These medications can cause serious side effects.)
- Assistive devices: Rehabilitative devices such as canes, walkers, wheelchairs, strollers and electric wheelchairs can help maintain your child's mobility and independence. Sometimes it helps to make modifications to your home, such as widening doorways and installing wheelchair ramps. Eventually, as respiratory muscles weaken, a child may also need the assistance of a breathing device (ventilator).
Treatment Options: Surgical
- Surgical release of contractures: A surgeon may cut through tendons to relieve contractures (tendon release surgery). Some surgeries can help a child continue to walk.
- Spinal fusion for scoliosis: Scoliosis in a wheelchair-dependent child with MD can become so severe it causes breathing problems and pneumonia. Having spine surgery before this happens can preserve breathing function, lessen back pain and improve sitting balance. All these factors improve the child's quality of life. The doctor may recommend surgery when the spinal curve reaches a certain size (i.e., more than 20 degrees). A surgeon opens up the child's back and inserts a metal rod into parts of the spine to help hold it in a straighter position (spinal fusion).
June 2004
All Information Copyright © American Academy of Orthopaedic Surgeons
www.aaos.org